Superbugs Could Become a Top Cause of Death by 2050
If left unchecked, antibiotic-resistant bacteria could kill more people than cancer by 2050
Antibiotic-resistant bacteria are no mere theoretical threat. In India last year, 58,000 children died of antibiotic-resistant infections. And in a new report conducted for the U.K. government, economist Jim O’Neill calculated that the global death toll to antibiotic resistant diseases could spike—to around 11 million deaths per year in the next 40 or so years, if things continue as they are.
Right now, says the BBC, roughly 700,000 people die from antibiotic-resistant diseases each year. A jump in the number of these deaths—to 10.7 million by 2050—would make these superbugs one of the biggest threats to human life, outpacing even cancer as a killer. Most of these deaths would be in Asia, the world’s most populous continent. But according to the BBC, North America would see approximately 317,000 deaths to antibiotic resistant diseases each year.
Constant fear over the next big killer—most of which never amounts to much—can leave some people feeling tired of the hype. After all, new diseases are new, and no one really knows how they’re going to shake out. Sometimes a disease grows into an epidemic like AIDS or one like Ebola; sometimes nothing much happens, if the disease burns out before it ever really gets going.
So it’s easy to ignore the CDC’s fretting over the emergence of so-called “nightmare bacteria”—deadly bacteria that are resistant to nearly every known class of antibiotics. But in the case of antibiotic resistance, the worry is real, and if steps aren’t taken soon to address the problem it could spell a disaster for the whole concept of modern medicine—the one we’ve known since the introduction of penicillin in the 1940s.
According to the BBC, the researchers on the new study suggest that their dire prediction is a conservative one: “The review team believes its analysis represents a significant underestimate of the potential impact of failing to tackle drug resistance, as it did not include the effects on healthcare of a world in which antibiotics no longer worked.”
[H/T Smithsonian]
Watch: Kevin Cole (UK) – Rise of the Superbug
from CIANT Prague
Antibiotic-resistant bacteria have become an increasingly dangerous and prevalent threat to the human race. Pathogens now termed as ‘Super-bugs’ have been created by humans through the use and overuse of antibiotics and now threaten our health and wellbeing. These superbugs appear to be evolving these resistance mechanisms at a faster rate than we can discover or create new antibiotics and we are forced to look to alternate methods to tackle and reduce infections.
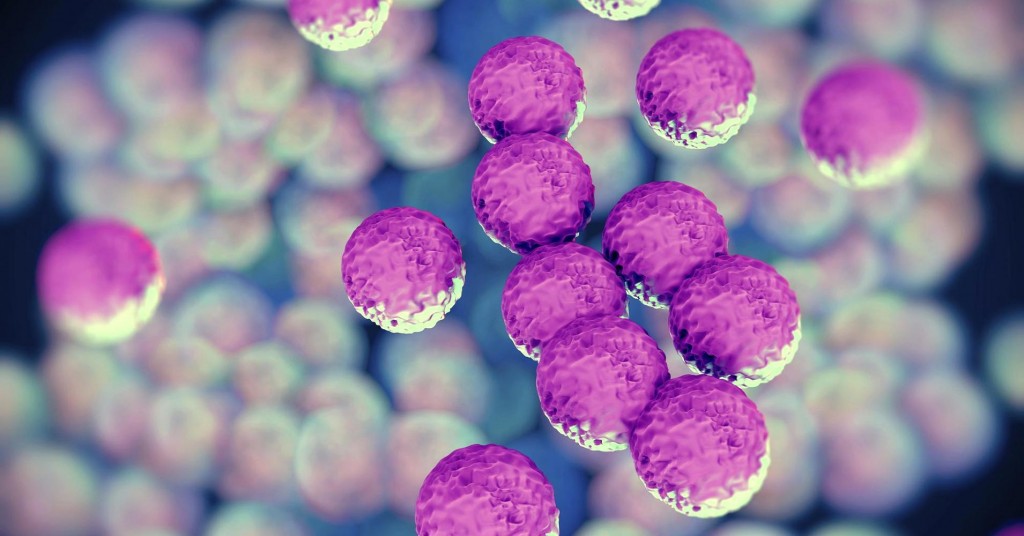
One of these; Methicillin-Resistant Staphylococcus aureus (MRSA) has now become a major global-healthcare issue. These bacteria can readily live on the skin of humans and in the environment. Certain strains are even suited to dwelling in hospitals amongst antibiotics and stringent cleaning regimens.
Hospital-acquired MRSA and S. aureus infection rates remain high even though they have been targeted by infection control policies as we still do not fully understand the exactly how they are transmitted amongst patients.
With the advent of Whole-Genome Sequencing (WGS) we may now be able to shed light on the exact routes these pathogens take when moving from patient to patient. WGS will allow us to discriminate between bacteria with such high resolution that we may be able to track and even prevent single isolates as they move through hospitals and communities.
We are using WGS alongside a range of conventional methods to attempt to take a snapshot of exactly how S. aureus is acquired by patients in a hospital ICU ward. By sampling patients, ward staff and the environment for S. aureus we hope to use WGS to linkup genetically identical isolates (i.e. the exact same organism) and use this information to identify and characterise exact ‘transmission events’. If we can determine exactly how S. aureus is passed from one patient to another then hopefully infection control interventions can be implemented that will stop the organism in its path.
As we gain greater understanding of how the genes we unravel translate to particular features of bacteria our ability to treat infections will improve. We are now moving to a scientific method whereby instead of merely seeing the phenotypes an organism may present we are now able to detect the genes that determine these phenotypes. WGS can be used not only detect any (potential) outbreaks of particularly contagious strains but also give us knowledge of antibiotic-resistant mechanisms or virulence factors that it may have. Perhaps the near future we may also be able to utilise this method to observe the bacterial evolution in real time so that we may be able to pre-empt potentially threatening mutants that will inevitably emerge.